What symptoms do patients with primary hyperparathyroidism have?
Many patients with primary hyperparathyroidism have no symptoms. However, the most common symptoms patients have are vague and can include chronic fatigue, body aches, difficulty sleeping, memory loss, poor concentration, depression and headaches.1
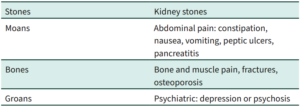
Only 20% of patients with primary hyperparathyroidism present with the classical symptoms of hyperparathyroidism that we were taught at medical school:
How do I diagnose primary hyperparathyroidism?
Request the following tests:
- Serum calcium (adjusted calcium) and phosphate
- PTH level
- Vitamin D level
- Creatinine and eGFR.
In hyperparathyroidism we see both a raised PTH level and a raised serum adjusted calcium level. It is important to exclude a secondary cause of hyperparathyroidism by checking the vitamin D level, creatinine and eGFR. Secondary causes of hyperparathyroidism include vitamin D deficiency and chronic kidney disease.
Once the diagnosis of hyperparathyroidism is made, I recommend referring the patient to either a surgeon who performs parathyroidectomy or to an endocrinologist.
How common is primary hyperparathyroidism?
The age-adjusted prevalence of primary hyperparathyroidism is approximately 200 per 100,000 in women and 100 per 100,000 in men. Therefore, in a GP practice, of 1500 patients, approximately two patients will have primary hyperparathyroidism.
What are the long-term complications of primary hyperparathyroidism?
Severe classical primary hyperparathyroidism is associated with an increase in mortality.
The long-term complications of primary hyperparathyroidism include kidney stones, kidney failure, osteoporosis and fractures. Some but not all reports have shown an association between even mild primary hyperparathyroidism and an increase in mortality from cardiovascular disease and cancer.
Which patients benefit from surgery?
Most symptomatic and asymptomatic patients benefit from surgery.
In the 2022 guidelines for Evaluation and Management of Primary Hyperparathyroidism2 the indications for surgery are:
- Serum calcium 0.25mmol/L above normal
- Skeletal involvement: bone mineral density by T score <-2.5
- Renal involvement
a. eGFR or creatinine clearance <60 mL/min
b. Kidney stones
c. Hypercalciuria woman >250mg per 24 hours, men >300mg per 24 hours.
4. Age > 50.
What is the role of imaging in the management of hyperparathyroidism?
Imaging plays no role in the diagnosis of primary hyperparathyroidism. Imaging (bone scan, renal ultrasound, CT scan of kidneys) plays a role in the assessment of the effects of primary hyperparathyroidism. Imaging (ultrasound, sestamibi, 4D CT, spect CT and MRI) often helps the surgeon to localise the site of the abnormal parathyroid gland prior to surgery.
What is the pathology of the parathyroid gland in primary hyperparathyroidism?
Approximately 85% of patients with primary hyperparathyroidism have an adenoma of one gland. Occasionally adenomas may involve two glands. The remaining 15% of patients with primary hyperparathyroidism have hyperplasia of all four parathyroid glands.
Rarely carcinoma of a parathyroid gland may be the cause of primary hyperparathyroidism.
Primary hyperparathyroidism is due to dysregulated growth of parathyroid cells and decreased expression of calcium-sensing receptors (CaSR) on the surface of parathyroid cells.
How successful is surgery for primary hyperparathyroidism?
Surgery for primary hyperparathyroidism is usually highly successful with many surgical series showing biochemical cure in 96%+ of patients with one operation.
Are there any other treatments for primary hyperparathyroidism?
Yes, asymptomatic patients with primary hyperparathyroidism that do not meet the above criteria are usually best managed conservatively with hydration, observation and frequent reassessment of their biochemistry (Ca,PO4, PTH, creatinine, eGFR). Medical treatment includes avoiding dehydration, maintaining dietary calcium between 800 and 1000mg daily, depending on gender and age, maintaining a normal vitamin D level, bisphosphonates for decreased bone mineral density and bisphosphonates and/or cinacalcet to reduce serum calcium if it is too high.
Take-home messages:
- Because primary hyperparathyroidism is often asymptomatic and has long-term health implications, it is recommended that serum calcium and PTH levels are included when routine blood tests are requested.
- Patients with vague symptoms such as tiredness, fatigue, insomnia, depressed mood, poor concentration or poor memory should be screened for primary hyperparathyroidism.
- Hyperparathyroidism is easily detected with the following blood tests: serum adjusted Ca, PTH, vitamin D, creatinine, eGFR.
- Refer patients with a high PTH level and a high calcium level to a surgeon who performs parathyroidectomy or to an endocrinologist.
References:
- Parathyroid.com
- Bilezikian JP, et al. Evaluation and Management of Primary Hyperparathyroidism: Summary Statement and Guidelines from the Fifth International Workshop. J Bone and Mineral Research 2022; 37:2293–2314.
- Ye Z, et al. The efficacy and safety of medical and surgical therapy in patients with primary hyperparathyroidism: A systematic review and meta-analysis of randomised controlled trials. J Bone and Mineral Research 2022; 37:2351–2372.
- Hall F. Primary hyperparathyroidism presenting as tiredness, fatigue and poor concentration. A curable condition. GP Voice August 2024.