Parotid Tumours and Salivary Stones
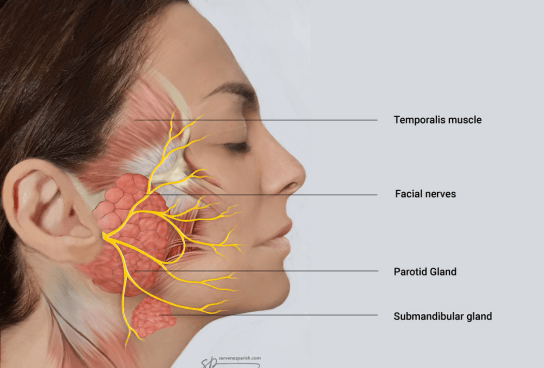
Your salivary glands make about 1.5 litres of saliva per day. Saliva is essential for the health of your mouth, throat and teeth. Saliva is a lubricant and helps food slide down your throat. Without saliva our teeth decay quickly. There are three pairs of big salivary glands on each side of your mouth, the parotid gland, the submandibular gland and the sublingual gland. The parotid gland lies in front of the ear, the submandibular gland lies under the jaw (mandible) and the sublingual gland lies under the tongue. There are hundreds of small salivary glands called minor salivary glands scattered throughout the mouth and throat.
The Parotid Gland:
The parotid gland lies in front of and below the ear. The saliva from the parotid glands is watery and drains inside the mouth at the back of the cheek. The facial nerve runs right through the parotid gland. This is an important nerve that divides into several branches that supply the muscles of the face.
The Submandibular Gland:
The submandibular gland lies under the jaw (mandible). It has a small duct (tube) that carries the saliva into the mouth and opens under the tongue in the midline.

What are the symptoms of a Salivary Gland Disorder?
As with most things, we take normal healthy salivary glands for granted until things go wrong. Salivary gland problems are not uncommon. Problems of salivary gland disorders include:
Drooling
Drooling is quite common in young children. Usually by the age of 4 to 5 years children stop drooling. Some children with developmental issues (for example, cerebral palsy) may keep drooling. Drooling can be socially embarrassing and isolating. For people that continue drooling, Botox injected into the submandibular glands or rerouting the duct of the submandibular glands (submandibular duct repositioning) usually helps.
Too little saliva (Xerostomia)
Too little saliva can be a devastating problem, resulting in bad breath, accelerated dental decay and a constant dry mouth, which can develop into a sore mouth. Chewing, swallowing and taste can also be affected.
Causes of a dry mouth include medications, radiotherapy and Sjogren’s syndrome. Many medications can cause a dry mouth including antidepressants, antihistamines, blood pressure medications, indigestion medications and others. Radiation treatment to the head and neck area frequently damages salivary glands. Sjogren’s disease is an autoimmune disease where the body attacks the salivary glands and the tear glands. Patients with this disease often complain of dry eyes and a dry mouth.
Infection of a salivary gland (parotitis)
Many of our patients wonder “how do you get a salivary gland infection?” Mumps is the most common viral infection of the parotid caused by the paramyxovirus. Infection of the parotid gland is commonly seen in adults and the elderly and is often associated with another illness (the flu or pneumonia). The parotid gland becomes swollen and tender. Usually, pus can be seen from the opening of the parotid duct inside the cheek. This is often due to the bacteria Staphylococcal aureus. Treatment for a parotid infection is prescribed antibiotics, plenty of fluids, pain medications and massaging of the gland to express the pus.
Blockage and swelling of a salivary gland (sialadenitis)
The parotid and submandibular glands both drain through small ducts (tubes) into the mouth. These ducts can be blocked by a salivary stone, a narrowing of the duct (stenosis) or thick secretions. This condition is referred to as sialadenitis.
Patients describe swelling of the affected gland which often comes on with eating. The swelling may last any time from 20 minutes to several days. Sometimes a sudden gush of salty fluid into the mouth is noted. Occasionally a salivary duct stone can be seen or palpated. Chronic sialadenitis symptoms include intermittent recurrent episodes of tender swelling.
An ultrasound scan or CT scan may detect a salivary stone or a narrowing of the salivary duct. Treatment of chronic sialadenitis often involves a procedure called sialendoscopy where a tiny telescope is inserted into the duct.
Miscellaneous salivary conditions
Sjogren’s syndrome is an autoimmune disease where the body attacks the salivary glands and the tear glands. Patients complain of dry eyes and a dry mouth.
Biopsy of a minor salivary gland and a blood test can confirm the diagnosis of Sjogren’s syndrome. The biopsy is taken from the lower lip. A small piece of tissue is removed from the lower lip.
Juvenile recurrent parotitis is an uncommon condition seen in children where there are episodes of recurrent swelling and pain in one or both parotid glands. Treatment is initially with antibiotics and pain medication. For recurrent or severe attacks, hydrocortisone or Lipiodol (an oil based iodine contrast agent), is placed into the duct of the parotid gland.
A ranula is a cystic swelling under the tongue or jaw. A ranula is due to leakage of mucus from the sublingual gland into the adjacent tissues. Treatment is removal of the sublingual gland.
A mucocele is due to leakage of mucus from a minor salivary gland. The lower lip is the most common site of a mucocele.
If you are experiencing any of the above-mentioned conditions with your salivary glands, please contact Dr Francis Hall. He will be happy to assist you and advise the next steps to take. Please contact us on (09) 281-2963 or book an appointment online.
Salivary Gland Disorder treatments
We understand that the thought of treatment or surgery can be overwhelming, but you are in safe hands. Dr. Francis Hall is an expert head and neck specialist and will carefully talk you through your options to treat your salivary gland condition.
Sialoendoscopy
Sialoendoscopy refers to an operation where a small telescope (sialoendoscope) is inserted up the duct of the involved gland to diagnose and treat the cause of the obstruction. Salivary stones can be removed during this procedure. Strictures can be dilated with the telescope, widening any narrow ducts in the process. Medications including steroids and Lipiodol can be placed into the duct of the gland to treat any inflammation. After dilation of a stricture a stent may be placed and removed a few weeks later. Recovery from sialoendoscopy is very fast-usually just a day to two.
If the salivary duct stone cannot be removed or the narrowing of the duct recurs, the involved salivary gland may need to be removed.
Parotid tumours
Tumours of the parotid salivary gland present as a lump just in front or below the ear. Tumours of the parotid gland are usually benign (not cancerous) but about 15% are malignant (cancerous). Signs of a malignant tumour (cancer) include a weak or paralysed face and enlarged lymph nodes in the neck. Sometimes malignant tumours are painful or grow rapidly. The most common benign tumours are a pleomorphic adenoma and Warthin’s tumour. About 5% of pleomorphic adenomas change and turn into cancer. Warthin’s tumours are usually seen in male smokers in their 70’s. The most common malignant tumours in the parotid gland are squamous cell carcinoma of the skin (skin cancer) that has spread to the parotid gland, mucoepidermoid carcinoma and adenoid cystic carcinoma.
Tumours of the submandibular salivary gland are a lot less common and about one third are malignant. Tumours of the sublingual salivary gland are rare and one half are malignant.
Tumours of parotid tumours are treated with an operation to remove the tumour (parotidectomy). For patients with malignant (cancerous) tumours, Dr. Hall presents the history and examination findings to the head and neck MDM (multidisciplinary meeting). The MDM is attended by radiologists, pathologists, surgeons, radiation oncologists and medical oncologists. All the investigations (CT, MRI scans and FNA) are reviewed and recommendations for treatment are made. Patients with high grade malignant tumours (adenocarcinoma, high grade mucoepidermoid carcinoma and metastatic squamous cell carcinoma from the skin) also require a neck dissection (see neck dissection section). Tumours of submandibular gland are treated with excision of the submandibular gland. Some patients with malignant (cancerous) tumours of the parotid gland or submandibular gland require radiotherapy after surgery.
To determine whether the lump in your salivary gland (parotid or submandibular gland) is either benign or cancerous, Dr Francis T. Hall will take a history and do a thorough examination including flexible endoscopy. Flexible endoscopy involves numbing the inside of the nose with local anaesthetic spray and inserting a tiny, flexible camera through the nose to evaluate the nose, throat (pharynx) and voice box (larynx). Additionally, an ultrasound scan of the lump will be performed. Dr. Hall will perform an ultrasound guided needle biopsy, fine needle aspirate (FNA) to collect a sample from the lump. This is a minor procedure, where a small needle is guided under ultrasound and a sample is collected. The sample is sent to a laboratory for testing. The report will be either benign or malignant. Surgery is recommended for most tumours including benign tumours. The most common benign tumour is a pleomorphic adenoma. Over time about 5% of pleomorphic adenomas turn into cancer and it is for this reason that surgery is usually recommended.
If you have a lump in one of your salivary glands, Dr. Francis Hall will be able to assist you. He has extensive additional training and experience in the evaluation and treatment of patients with tumours of the salivary glands. He runs a neck lump clinic which includes history, examination, flexible endoscopy, ultrasound and ultrasound guided FNA. Please contact us on (09) 281-2963 or book an appointment online.
Salivary Gland operations
Parotidectomy (parotid gland surgery)
This is the name given to removing all or part of the parotid gland. Patients with tumours of the parotid gland are treated with parotidectomy. Some patients with recurrent infections of the parotid gland are also treated with parotidectomy. The surgery is done under general anaesthesia so you will be fast asleep. An incision is made immediately in front of the ear in a skin crease. This incision continues either onto the upper part of the neck or behind the ear. The tumour is dissected off the branches of the facial nerve. A small plastic drain is placed. The incision is closed with a dissolvable suture placed deep to the skin. The drain is removed two days later. Complications are uncommon and include permanent weakness of a part of the face, a temporary collection of saliva (sialocele) under the skin, leaking of saliva through the skin (salivary fistula) and Frey’s syndrome. Frey’s syndrome is sweating of the skin in front of the ear when eating (gustatory sweating). Fortunately, Botox injected under ultrasound guidance is excellent treatment for a sialocele, salivary fistula and Frey’s syndrome. (see section under ultrasound)
Excision of Submandibular Gland
Patients with tumours of the submandibular gland are treated with excision of the submandibular gland. Some patients with recurrent infections or stones (calculi) within the submandibular gland itself also may need the submandibular gland excised. The surgery is done under general anaesthesia so you will be fast asleep. An incision is made in a skin crease under the jaw. The submandibular salivary gland is removed. A small plastic drain is placed and the incision is closed with a dissolvable suture placed deep to the skin. The drain is removed the following day. Complications are uncommon and include injury to adjacent nerves. The adjacent nerves are the marginal mandibular branch of the facial nerve which pulls the lower lip down, the lingual nerve that supplies taste and general sensation to the side of the tongue and under the tongue and the hypoglossal nerve that moves the tongue.
Dr. Hall and Salivary conditions:
Dr. Francis Hall is a fellowship trained head and neck surgeon with extensive experience in the treatment of both benign and malignant tumours of the salivary glands. He was the first in New Zealand to perform sialoendoscopy and after two years of performing sialoendoscopy, presented his results at the New Zealand Society of Otolaryngology Head and Neck Surgery Annual Scientific Meeting in 2010. In 2016 he was also the first in New Zealand to use the stone breaker, an endoscopic pneumatic lithotripter used to break up larger stones. In 2018 , Dr. Hall was the first in New Zealand to use Lipiodol to treat certain salivary disorders. He presented their results on using Lipiodol to treat juvenile recurrent parotitis at the annual audit day of the Department of Otolaryngology Head and Neck Surgery at Auckland Hospital in May 2019 and at the Rotorua GP CME annual conference in June 2019.